Table of Contents
What Happens Beneath a Missing Tooth
Scenario 1: Your Adjacent Teeth Are Pristine
Scenario 2: Speed Takes Priority
Scenario 3: Bone Health Limits Your Options
Scenario 4: Cost Now vs. Cost Over Time
Scenario 5: Replacing Multiple Teeth at Once
Additional Factors That Can Influence the Decision
How Dentists Weigh the Final Choice
Getting a Clear Recommendation
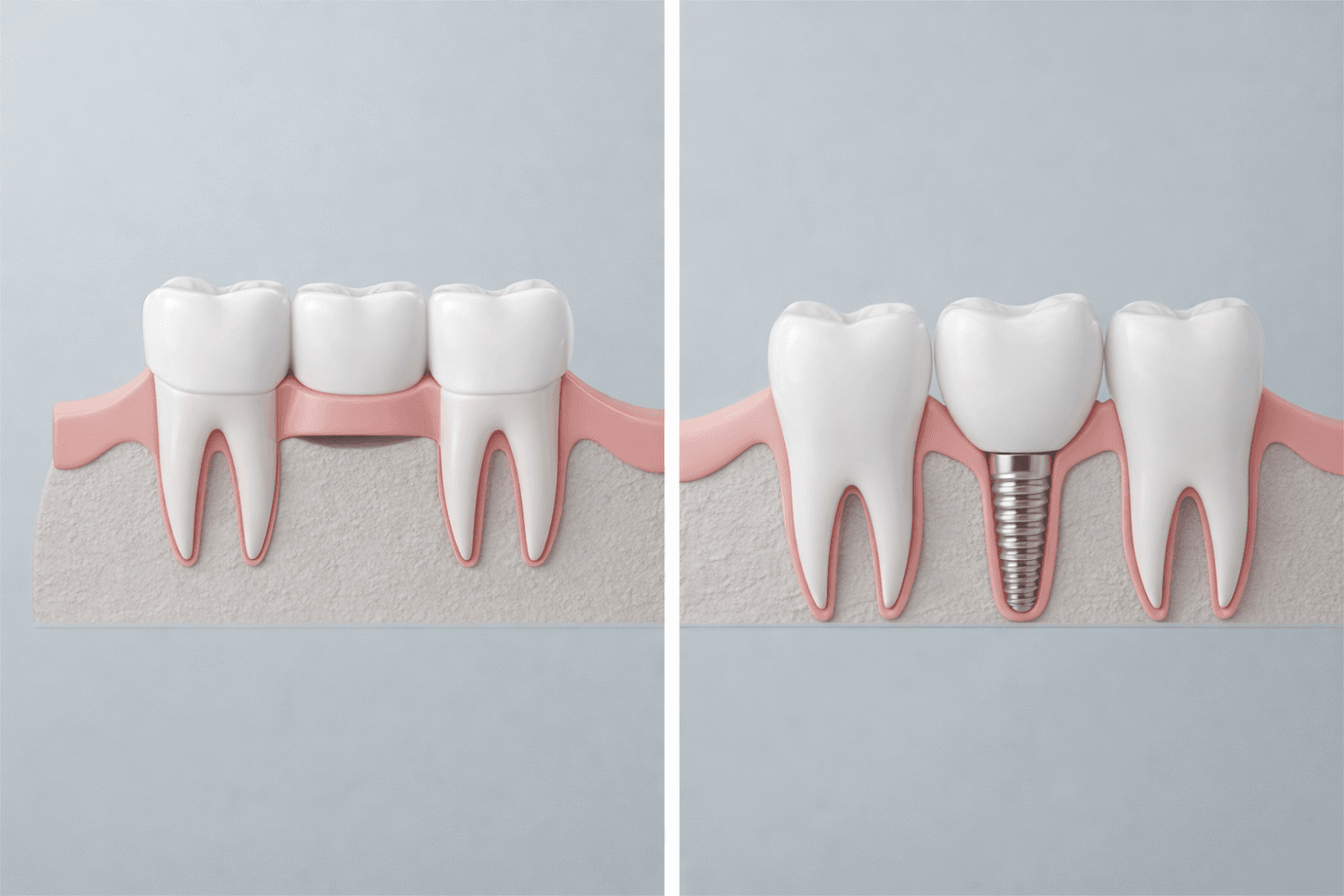
You know the difference between a dental bridge and a dental implant. On paper, the dental bridge vs. implant decision can seem straightforward. One replaces a missing tooth by anchoring to the teeth beside it. The other replaces the tooth and its root.
That clarity disappears once you’re looking at your own treatment plan. Both options solve the problem, but they solve it in very different ways. One avoids surgery but alters healthy teeth. The other preserves neighbouring teeth but requires more time, healing, and planning.
Most advice online stops at surface-level comparisons. Cost versus longevity. Speed versus durability. Those lists leave out many factors that drive the decision in real cases.
Dentists don’t choose between a dental bridge or implant based on preference. The decision depends on anatomy, bone health, timing, budget, and how the surrounding teeth are already holding up. When those details are weighed together, the better option often becomes clear.
What Happens Beneath a Missing Tooth
When a tooth is lost, changes begin beneath the surface. Without a tooth root in place, the jawbone no longer receives the stimulation it needs to maintain its volume. Over time, the alveolar bone, the part of the jaw that supports the teeth, begins to shrink. Studies show that bone width can decrease by as much as 25 percent within the first year after a tooth is lost.
That detail shifts the decision between a dental bridge and an implant in an important way. The question is no longer just how to replace a visible tooth, but whether the underlying bone is being preserved or allowed to deteriorate.
A dental bridge restores appearance and function. Chewing and speaking return to normal. Beneath the gum line, however, the bone continues to resorb because nothing is replacing the missing root.
A dental implant functions differently. By anchoring directly into the jaw, it replaces both the tooth and the root. This ongoing stimulation helps maintain bone volume and supports the surrounding structures.
Bone preservation is one factor, not the deciding factor on its own. In the dental bridge vs. implant discussion, it needs to be weighed alongside timing, cost, and the condition of surrounding teeth.
Scenario 1: Your Adjacent Teeth Are Pristine
If a tooth is lost due to localized trauma, such as an accident, and the teeth on either side are healthy and untouched by decay or restorations, the decision often leans in one direction.
In this situation, an implant is usually the stronger option.
Placing a dental bridge requires removing enamel from the neighbouring teeth to support the crowns that hold the bridge in place. That turns a single missing tooth into a restoration that involves three teeth. Once healthy enamel is removed, it cannot be replaced.
Choosing a bridge in this scenario means relying on two healthy teeth to support the replacement. If decay or complications develop in either anchor tooth later on, the stability of the entire bridge is affected.
When the surrounding teeth are healthy, preserving them matters. An implant replaces the missing tooth without altering adjacent teeth and functions as a standalone solution.
Scenario 2: Speed Takes Priority
In some cases, timing matters more than long-term durability. When a missing tooth needs to be replaced quickly, the treatment timeline becomes a deciding factor.
Dental implants require healing at multiple stages. If bone grafting is needed, healing can take several months before the implant is even placed. After placement, the implant must integrate with the bone before a crown can be attached. From start to finish, the process often spans six to ten months, and not every patient qualifies for same day or immediate load options.
A dental bridge follows a much shorter timeline. The adjacent teeth are prepared, impressions are taken, and a temporary restoration is placed. Within a few weeks, the permanent bridge is cemented, restoring function and appearance without extended healing.
When speed is the priority, a bridge often provides the most predictable path forward. It delivers a stable result under a tight timeline, even though it may not offer the same extended benefits as an implant.
Scenario 3: Bone Health Limits Your Options
Bone volume plays a central role in whether an implant is feasible. When a tooth has been missing for several years, the jawbone in that area may no longer have enough density to support an implant on its own.
In cases of insufficient bone, implant placement often requires additional procedures such as bone grafting or a sinus lift for upper teeth. While these procedures are common and generally safe, they increase cost, add surgical complexity, and extend the overall treatment timeline by several months.
Healing capacity also matters. Conditions such as uncontrolled diabetes, smoking, or other medical issues that impair healing can reduce the likelihood of successful bone integration. Implant failure rates are higher in smokers, particularly when grafting is involved.
When bone volume is limited or healing potential is compromised, a dental bridge is often the more practical choice. A bridge relies on the adjacent teeth for support rather than the jawbone, allowing treatment to move forward without additional surgery.
Scenario 4: Cost Now vs. Cost Over Time
Cost plays a role in nearly every treatment decision, and tooth replacement is no exception. The difference between a bridge and an implant is not just the price on the day treatment begins, but how that cost plays out over time.
A dental bridge typically has a lower upfront cost, and insurance coverage often favours it. Many plans cover a higher percentage of bridge treatment, while implant placement may receive limited coverage or none at all beyond the crown. For patients working within a strict budget, a bridge can restore function without the higher initial expense.
Longer-term considerations tell a different story. Dental bridges have a finite lifespan, commonly lasting five to fifteen years. Over time, decay, gum recession, or wear on the supporting teeth can require the bridge to be replaced, sometimes more than once.
Dental implants follow a different pattern. Once the implant integrates with the bone, it is designed to last for decades. While the crown may need replacement due to wear, the implant itself is typically permanent.
The distinction is not about right or wrong, but timing. A bridge often makes sense when immediate affordability is the priority. An implant may offer greater long-term value when upfront cost is less restrictive. Both are valid solutions when chosen with a clear understanding of their financial implications.
Scenario 5: Replacing Multiple Teeth at Once
Replacing several missing teeth introduces different mechanical considerations. When three or more teeth are missing in a row, both traditional bridges and individual implants come with tradeoffs.
Placing an implant for every missing tooth can be costly and is not always necessary. On the other hand, using a traditional bridge to span a long gap places significant stress on the supporting teeth. As the span increases, more force is transferred to the anchor teeth, which raises the risk of fracture or failure over time.
An implant-supported bridge offers an alternative. In this approach, implants are placed at strategic points along the gap, and a bridge is attached to them rather than to natural teeth. This provides stability while reducing the number of implants required.
By relying on implants instead of neighbouring teeth for support, this approach helps preserve bone and limits stress on natural teeth. It often balances strength, longevity, and cost more effectively than either option alone when multiple teeth are missing.
Additional Factors That Can Influence the Decision
Daily Cleaning and Maintenance
A dental bridge and a dental implant differ in how they are cleaned. Bridges require additional tools, such as floss threaders or specialized brushes, to clean beneath the false tooth. If plaque accumulates around the supporting teeth, the risk of decay or gum disease increases over time.
Dental implants are cleaned more like natural teeth. Brushing and flossing follow a familiar routine, which can be easier for patients with limited dexterity or inconsistent hygiene habits. Daily maintenance does not determine eligibility for either option, but it can influence long-term success.
Comfort With Surgery and Healing
Surgical treatment is a concern for many patients, even when they are medically good candidates. Dental implants involve a surgical procedure, while bridges do not.
Recovery experiences vary, but discomfort after implant placement is often comparable to or less than that of a tooth extraction. Bridge placement avoids surgery but can lead to temporary sensitivity in the supporting teeth due to enamel removal.
Comfort level with surgical treatment can affect follow-through and satisfaction. While it does not override clinical factors like bone health or stability, it plays a role in choosing a treatment plan that a patient is willing and able to complete.
How Dentists Weigh the Final Choice
In the dental bridge vs. implant decision, recommendations are shaped by patterns seen across anatomy, healing capacity, and stability across time. These factors often carry the most weight in clinical decision-making.
A dental bridge is more often recommended when:
- Bone loss limits implant placement and grafting is not feasible or appropriate
- Adjacent teeth already require crowns or large restorations
- A shorter treatment timeline is necessary
- Insurance coverage significantly favours bridge treatment
- Medical conditions reduce healing capacity or increase surgical risk
A dental implant is more often recommended when:
- Adjacent teeth are healthy and free of restorations
- Hygiene and maintenance simplicity are priorities
- Preserving the jawbone and surrounding structures is a key concern
- The patient can accommodate a longer treatment timeline
- Long-term durability is prioritized over upfront cost
In some situations, a bridge is placed with the intention of transitioning to an implant later. This approach can be reasonable, but it comes with tradeoffs. Bone loss continues beneath a bridge, which can make future implant placement more complex and may require grafting that would not be necessary earlier.
How Dental Bridges and Implants Typically Compare
Getting a Clear Recommendation
Frameworks are helpful, but they can’t replace a clinical exam. Bone height, sinus position, and bite forces all influence whether a bridge or implant is appropriate, and those details require imaging to evaluate properly.
An in-person assessment allows those variables to be reviewed together and placed in context. With the right imaging, it becomes clear whether your anatomy supports an implant or whether a bridge is the more predictable option.
If you’d like to discuss your options, schedule a consultation at Somerset Dental on James. We’ll review your imaging and explain which approach makes sense for your situation.